A combination of interventions to reduce premature births prior to 34 weeks of gestation
Rodolfo de Carvalho Pacagnella
In pregnancy, the cervix functions as a “gate” that separates the baby from the external environment. When it opens, which should only occur at the time of delivery, it shortens. But in some cases, this shortening happens prior to delivery. The reasons why the phenomenon occurs are not fully understood, but what is known is that it is linked to an inflammatory process that decreases the amount of collagen in the cervix, making it thinner. According to a 2014 Unicamp study, which followed 33,000 women in the South, Southeast and Northeast regions of Brazil, this process is involved in about 64.6% of spontaneous premature births.
This study, “Progesterone and cervical pessary to prevent premature birth or P5 study,” led by researcher Rodolfo de Carvalho Pacagnella, professor in the Department of Tocogynecology at Unicamp’s School of Medical Sciences, aimed to identify and halt the shortening process before early labor.
The team recruited about 20,000 women and collected data from more than 9,000 women between 18 and 23 weeks pregnant in 17 hospitals tied to the Unified Health System (SUS) across Brazil. In these centers, the research team utilized transvaginal ultrasound devices to assess pregnancy and measure the cervix.
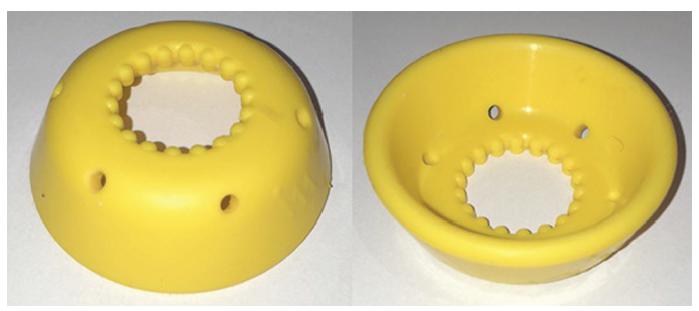
Pregnant women who agreed to participate in the research received the exam, which is not offered in the regular prenatal care in Brazil, free of charge. If no changes in cervical length were identified, the pregnant women were advised to continue with their regular prenatal care. If a shortening of the cervix was detected, the woman received special monitoring to avoid premature labor. All participants with cervical shortening received a 200-milligram capsule of progesterone and some, chosen at random, also received a pessary, a silicone ring, to close the cervix and reduce the possibility of premature birth. Both were inserted into the vagina until the end of pregnancy. The team also regularly monitored participants until delivery.
“Our goal was to assess whether the combination of progesterone and a pessary was more effective than just the hormone in reducing the chances of premature birth,” says Pacagnella. Of the 9,000 women followed, 936 were diagnosed with a short cervix (less than 30 millimeters) and received one of two interventions detailed above.
The combination of pessary plus progesterone is not superior to progesterone alone in reducing the occurrence of serious complications for premature babies, but the two combined treatments greatly reduced the chances of delivery before 34 weeks of gestation, an age when complications for the baby are more severe. The paired treatment also decreased severe and extreme premature births (born at less than 28 weeks), the length of hospital stays for babies, and the use of medications.
Research has also shown that combined pessary + progesterone treatment was beneficial to women who were pregnant for the first time (nulliparous), had a cervix under 25 millimeters and were gestating a single baby. Among these pregnant women, there was a reduction in both prematurity and adverse effects on the newborn. On average, children of mothers who used the pessary were born one week later (37 weeks) than those who used progesterone alone (36 weeks). The frequency of premature babies was also lower among those who used the silicone ring (29%), as compared to just the medication (39%). “However, we still need more studies to convert the findings into recommendations or protocol,” highlights Rodolfo.
By evaluating 9,000 women, the researchers were able to establish the first Brazilian curve on cervical length. Due to this, researcher found that the cervical size of Brazilian women is different from other populations. This difference could be important in determining which women are at risk of premature birth.
The researchers also mapped the risk factors and protective factors for a short cervix. These include uterine inflammation, cervical surgery and previous premature births (mainly below 28 weeks), abortions, low weight of the mother (doubles the risk) and, for women who have already had children, high education. The protective factors include obesity, as it is usually related to longer cervixes, and previous childbirths.
In addition to the scientific results, the study also developed new protocols and public policies. Because of the study, the city of Jundiaí (SP), which participated in the research by recruiting women, instituted transvaginal ultrasound and cervical measurement as mandatory exams during prenatal care. “When Professor Rodolfo invited the Faculty of Medicine of Jundiaí (FMJ) to participate in the project, we realized that the challenge would be immense and that the best way forward was to encourage the public sector that serves pregnant women to institute policies that universalize the measurement of the size of the cervix in prenatal care throughout the municipality,” according to Professor Rodrigo Camargo of FMJ. “The strategy was well-accepted, and it works today, even after the end of the research.” According to Pacagnella, it was an unexpected result, but extremely important for public health. Another innovation was the satisfaction survey provided to all participating women. “I went through three premature births, and doctors identified that I had a shortened cervix, which made it difficult to carry the baby during pregnancy,” says one study participant. “When I got pregnant again, I agreed to undergo treatment with a pessary. It worked. The ring was removed at 37 weeks and I got my baby at 38 weeks, within the normal time frame.”

